Infertility

Infertility is a major problem today. As recently as 1980 only an estimated 10 to 15 % of couples were affected. Now most surveys put the percentage of couples remaining childless involuntarily at above 20% in developing countries.
Infertility is defined as inability to conceive after a year of regular unprotected intercourse. Most couples are advised to seek help after trying for a year but some with more complex or pre-existing problems are advised to do so earlier.
Fortunately, medical advances have come up with answers to most infertility problems. If you have time the sites below (at end of page) are recommended as they give commendable advice. Only mainstream and credible sites are recommended to save you poring thru too much frivolous information.
Most doctors wisely advocate a comprehensive approach to investigating and treating infertility. IVF should only be considered if there is a definite reason. Most couples (about 70%) who seek treatment get pregnant without having to go for IVF.
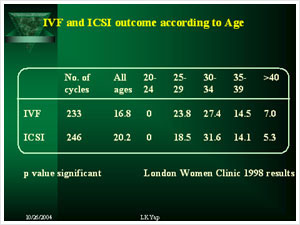
To give you an idea what is available skip to the discussion of tests available. However, should IVF be needed it should be attempted at a reputable center early. Note that IVF /ICSI results drop after age 35 (below)
Some of the more common investigations are:
- Blood tests
- Vaginal swabs
- Semen analysis
- Semen cultures
- Ultrasound scans
- Hysterosalpingography (HSG)
- Hysteroscopy
- Laparoscopy
| Follicle stimulating hormone (FSH) | - | measured during the early part of the menstrual cycle (day 2 to 5) gives an indication of the quality and number of eggs available if ovulation induction is needed |
| Luteinising Hormone (LH) | - | as for FSH |
| Estradiol (E2) | - | an estrogen which is low between day 2 to 5 but rises later in the cycle |
| Prolactin | - | high levels may indicate lack of egg production or that eggs may be of poorquality |
| Progesterone | - | this hormone peaks a week before menstruation and high levels indicatethat ovulation (release of an egg) has occurred |
| Thyroid hormones | - | may be useful as under or over activity of the thyroid gland makes pregnancy difficult to achieve |
| Full blood counts | - | occasionally these are needed to assess the woman general health |
| Rubella IgG titres | - | it is useful to have a woman's immunity to rubella assessed. Contacting rubella in early pregnancy can give rise to severe deformities in the unborn child, undergoing under a pregnancy blood test my help. It is prudent to get protected before trying to get pregnant |
| Hepatitis B Antibodies | - | these are required if assisted conception is planned |
| Hepatitis Antigen | - | these are required if assisted conception is planned |
| HIV | - | these are required if assisted conception is planned |
High vaginal swabs taken to check for pathogenic bacteria are useful. Often mild infections cause difficulty in conceiving.
PAP smears may be helpful in picking up yeast infections and HPV.
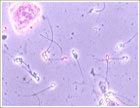
It takes two to tango. The main contribution from the male partner is sperm . An early assessment is extremely useful.
 |
A typical view of sperm under the microscope |
 |
Enlarged view of an abnormal sample |
Undetected infections do result in ineffective sperm and if detected need treatment.
Abdominal ultrasound scans with a full bladder give useful information about the ovaries, uterus and possibly the fallopian tubes.
Vaginal ultrasound examinations are more uncomfortable but give much more detailed information about the female organs. Most gynecological problems are detectable by this method. A serial scan is sometimes necessary to determine if egg formation is normal.
An X-ray is taken of the uterus after a dye in injected. This shows if the tubes are patent or blocked. A typical picture of a normal uterus with patent tubes is shown below.
The hysteroscope allows a careful and direct inspection of the inside of the uterus. Adhesions, polyps and fibroids which may make it difficult for the fertilized egg to attach may be detected and treated through a hysteroscope.
Picture of hysteroscopy being done
 |
Normal view on hysteroscopy |
Laparoscopy is a more invasive procedure but gives a good view of the pelvis allowing close inspection of the ovaries, tubes and uterus. Problems detected during laparoscopy can be treated at the same sitting. Laparoscopy may be the only means of detecting adhesions, mild to moderate, endometriosis, tubal or uterine abnormalities and subtle problems of the pelvis.
Some doctors have questioned the value of laparoscopy but it is best you judge for yourself. In a recent paper: A selected group of patients unable to get pregnant while on clomiphene, and with a normal hysterosalpingogram underwent diagnostic laparoscopy, Out of 92 women :
- 35 percent of the participants had a positive laparoscopy,
- 29 percent had stage I or II endometriosis
- 33 percent had a normal pelvis
2 thirds proved to have needed the investigation.
Is laparoscopy needed during infertility evaluation?
Fertility and Sterility 2003; 80: 1450-3
The operation is relatively simple but as in all operations there is a small risk of damage to internal organs and anesthetic problems.
- Ovulation Induction
- Intrauterine Insemination
- IVF
- ICSI
- Embryo freezing
- MESA / TESA
- Blastocyst culture
Some women do not ovulate (produce an egg) regularly or sometimes not at all. Normally a woman produces an egg a month in the middle of the menstrual cycle.
Where there is difficulty in producing an egg regularly, medication can be given to induce (hence the term induction) a woman to produce an egg. The problem with most of these treatments is that more than one egg can be produced as a result. This can result in multiple pregnancies, a situation the newspapers may like but can be dangerous to the mother as well as babies.
Occasionally, hyperstimulation may occur. This is a high risk situation and should be prevented. To ensure safety as well as to ensure that a response occurs, ovulation induction should be monitored by ultrasound scan. This checks on the number and size of follicles.
Common medications used are clomiphene citrate (Clomid), tamoxifen, human menopausal gonadotrophins, and purified follicular stimulating hormones (FSH).
is the simplest and is used as first line treatment. The usual starting dose is 50 mg. daily for 5 daysn from day 2 to 6 of a menstrual cycle. Some regimes call for a day 5 start, ending on day 9.
The dosage is increased if no eggs are produced. Dosage should not exceed 150 mg daily.
is a combination of hormones collected from menopausal women's urine. It has been purified and is potent in stimulation of the ovary to produce eggs.
is a recent development with a more specific and highly purified hormone FSH being made by recombinant technology. This is especially in polycystic ovarian disease where ovulation is infrequent.
During this procedure semen is first collected from the husband, treated in the laboratory to collect only the most active sperm. The treated sperm is then introduced into the uterine cavity (hence the term intra-uterine), past the cervix. This helps to get sperm nearer to its target, the oocyte (egg) which is being released from the ovary and starting its journey down the fallopian tube.
The timing of the procedure is important. Success is maximized by introducing the sperm just before the egg is released. To estimate the time of egg release (ovulation) we monitor the cycle with a combination of Ultrasonography and urine testing.
During an IUI cycle an average woman (someone who has a 28 day menstrual cycle) is scanned between day 10 to 12. The follicle size should be around 14mm. It is estimated that the follicle reaches an average size of 18 to 20 mm before it reaches maturity and is released as part of the ovulation process.
If the follicle size reaches 14 mm or more the urine is tested daily (or twice a day for greater precision). Once LH is detected in the urine ovulation is likely to occur within 24 to 36 hours.
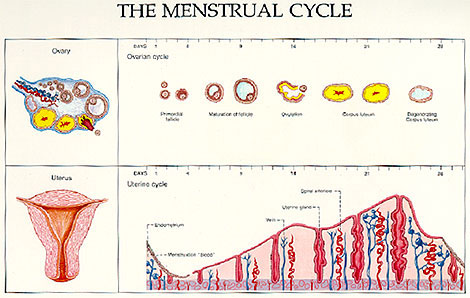
| Average cycle | - | Length 28 days. |
| - | Ovulation is usually on day 14 plus or minus 1. | |
| - | Follicle size before release of egg is 18 to 20 mm. | |
| - | Endometrium reaches a thickness of 8 to 10 mm. | |
| - | The brain releases a surge of luteinising hormone (LH) to start a process of maturation and about 36 to 40 hours later the egg is released (ovulation). LH is detected in the blood almost immediately on release. It (LH) appears in the urine several hours later. | |
| - | After ovulation the lining of the follicle undergo change and forms a corpus luteum. | |
| - | After ovulation the endometrium changes character and enters the secretary phase during which nutrients are released to nourish any developing embryo that may be trying to attach to the endometrium (implant). | |
| Natural cycle | - | The above description is during a natural cycle when usually only one egg is released. https://www.asrm.org/Patients/faqs.html |
| Stimulated cycles | - | To ensure better results it may be necessary to induce the ovary to produce more than one egg during the cycle. This can be achieved with clomiphene (Clomid) tablets, or injections with follicle stimulating hormones (FSH) in its natural form (HMG) or purified form (Puregon, Gonal F). These cycle tend to produce more than one egg and careful monitoring is necessary to prevent hyperstimulation which can result in great discomfort and danger to the woman, or produce multiple pregnancies. |

This is a service of the U.S. National Library of Medicine and the National Institute of Health. The most relevant information about cysts.
https://medlineplus.gov/ovariancysts.html

National Institutes of health
For more information about Infertility consult to our Singapore Gynae clinic.
